One of the essential skills of health educators is the ability to communicate easily with different groups and to explain complex health issues in easy to understand terminology,Thus definition of health promotion is like the process that empowers people to have more control over and improve their health, and allows themselves to redefine health, It’s always a question of “achieving a state of complete physical, mental and social well-being” “a community must be able to identify and realize its ambitions, satisfy its needs and transform its environment or adapt to it “this promotion campaign is useful in many cases such as illnesses social life or even sexual orientation such as LGBT target audiences need care that must be “scientifically valid and socially acceptable, universally accessible to individuals and families affected, at a cost these communities can provide in the areas of health.
10th globale health conference
HEALTH PROMOTION VIDEOS
Thinking about this situation and how I can use my skills as a health educator to teach about health issues and also find solutions to this issue that require medical treatment.
EMY:” I’m transgender since my parents know that,i I have got a several difficulties, like I’m no longer part of my family no one wants to talk to me, even at university other students always look at me through, many times I made attempts to commit suicide”
there are indeed two opposing models of society.
The principles of solidarity, the fight against inequalities, respect for the diversity of choices ,and health promotion requires a number of prerequisites and resources: peace, housing, education, food, income, a stable ecosystem, sustainable resources, social justice and equity.
Health promotion requires first conditions rather than preconditions.
Three principles are then set out:
• Health is a good investment because it enables social, economic and individual development. And you have to convince everyone of that.
• Health promotion is about health equity.
• Health prerequisites and goals cannot be achieved by the health sector alone. Health promotion requires the coordinated action of all concerned: governments, local authorities, different sectors of society (health, social, economic), associations, industry, the media, as well as actions at work to promote health,
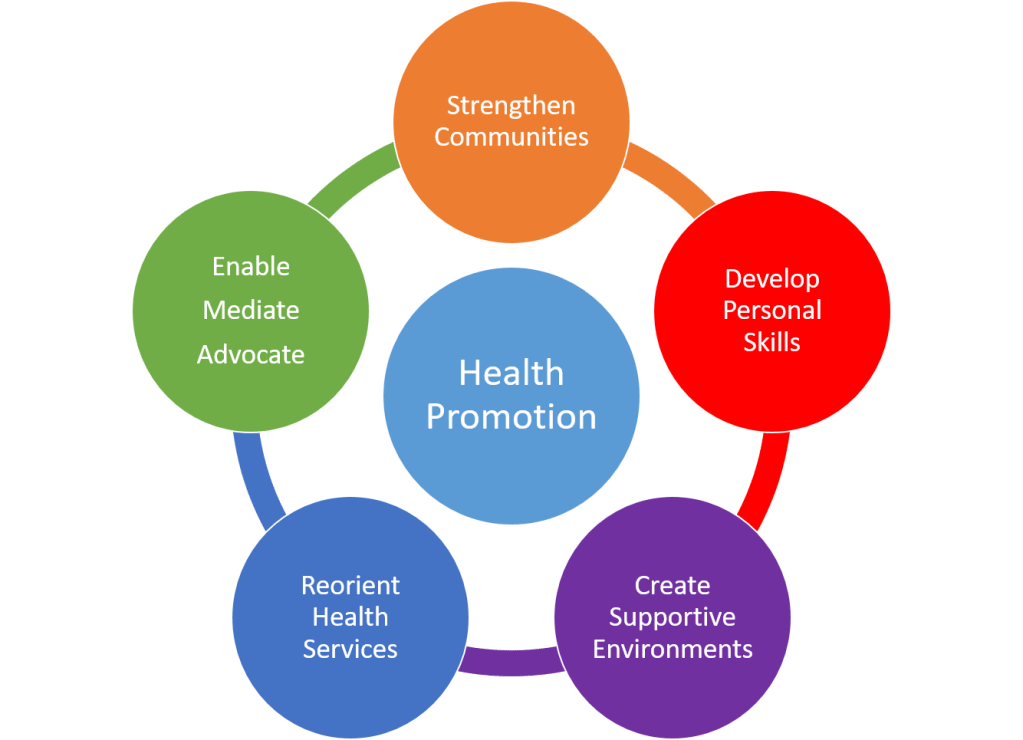
In five areas:
● Politics: health promotion must lead every political leader, at a level and in whatever sector he intervenes, to become aware of the consequences of his decisions on the health of the population.
● Environment: It is about motivating every person, every community, every region, every country to collectively conserve natural resources and create health-promoting relationships and living and working conditions.
● Democracy: Communities are seen as capable of taking charge of their destiny and taking responsibility for their actions.
● Health Education: This is about enabling people, at all ages, to acquire and strengthen life skills, including those that will enable them to participate in health promotion.
●Health services: that it is in fact a question of reorienting the services, of creating a system of care which best serves the interests of health, which is part of a logic of health promotion, which respects in particular the cultural and social dimension of people, which encourages and takes into account the expression of individuals and groups on their health expectations.
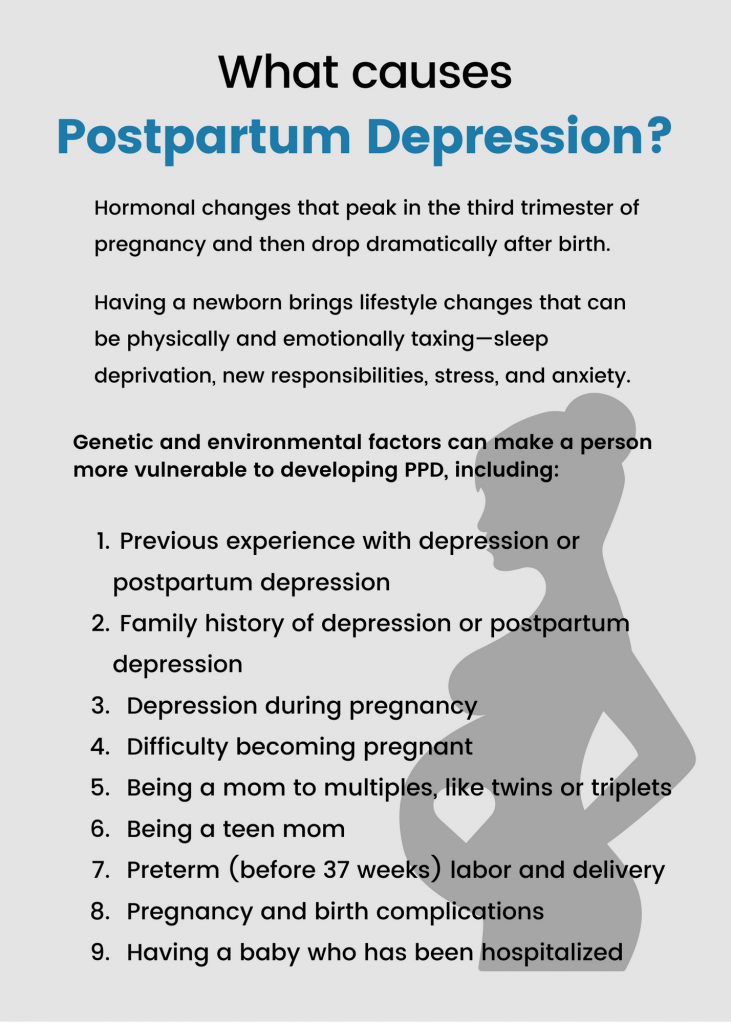
By respecting these principles, it seems that we can decrease the number of disparities persons each year,the dangers are always there, it’s not just the promotion of health but also a struggle to be responsible individually which explains the difficulties that can be encountered a health educator.
The most common health promotion is the community or public health framework, as a specific element of almost all public health systems, health education has found a strong and permanent home,however, many community service organizations and nonprofits employ health educators who spend time reviewing health data from the community, collecting information from focus groups or surveys and plan interventions that prevent or slow health problems that affect people where they live, typically write grant applications to implement their program plans.
Health educators in this context focus primarily on this health by educating the population on certain health topics and reducing high-risk behaviors such as suicide. people maintain mental, physical, and health safety. The health educator should visit with the company’s human resources representative and discuss recruitment on the program plan for a global health care.

HERE OTHER SOURCES ON HEALTH PROMOTION
https://health.gov/healthypeople/objectives-and-data/browse-objectives/lgbt/reduce-suicidal-thoughts-transgender-students-lgbt-d02
https://health.gov/healthypeople/search?query=Health%20Promotion%20
https://www.who.int/health-topics/health-promotion#tab=tab_1
https://www.who.int/westernpacific/about/how-we-work/programmes/health-promotion
https://www.vichealth.vic.gov.au/media-and-resources/vce-resources/defining-health-promotion
https://www.sciencedirect.com/topics/psychology/health-promotion
rachellepierre71@gmail.com