Maternal mortality is still very high in most underdeveloped countries the majority of these maternal deaths are due to late or inappropriate treatment
obstetric complications, to remedy this situation it is obvious to implement interventions that aim to improve the management of obstetric emergencies in low-resource countries. These interventions generally consist of mobilizing
communities to improve the use of care in a timely manner and to improve the care chain and medical practices at the different levels of the health pyramid. Such as: telemedicine, a
journal-based approaches a. Emergency consultation according to symptoms and avoid cases of maternal mortality or morbidity due to lack of assistance, and more effective interventions
positive about maternal and newborn health.
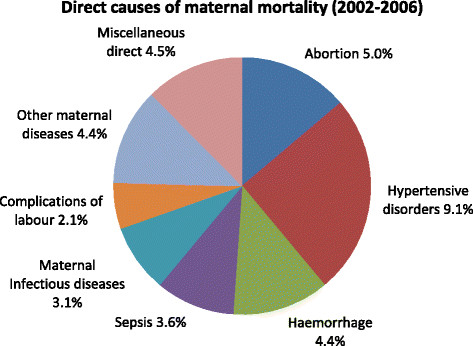
Uterine ruptures, ante- or postpartum haemorrhages, severe hypertension, infections and complications of the first trimester of pregnancy (abortion and ectopic pregnancy) are the cause of 80% of maternal deaths.
NON-MEDICAL CAUSES OF MATERNAL MORTALITY
For multiple socio-cultural reasons, home birth is still a common practice in traditional societies. Currently in the world, two-thirds of births take place at home and half are not
assisted by qualified personnel.
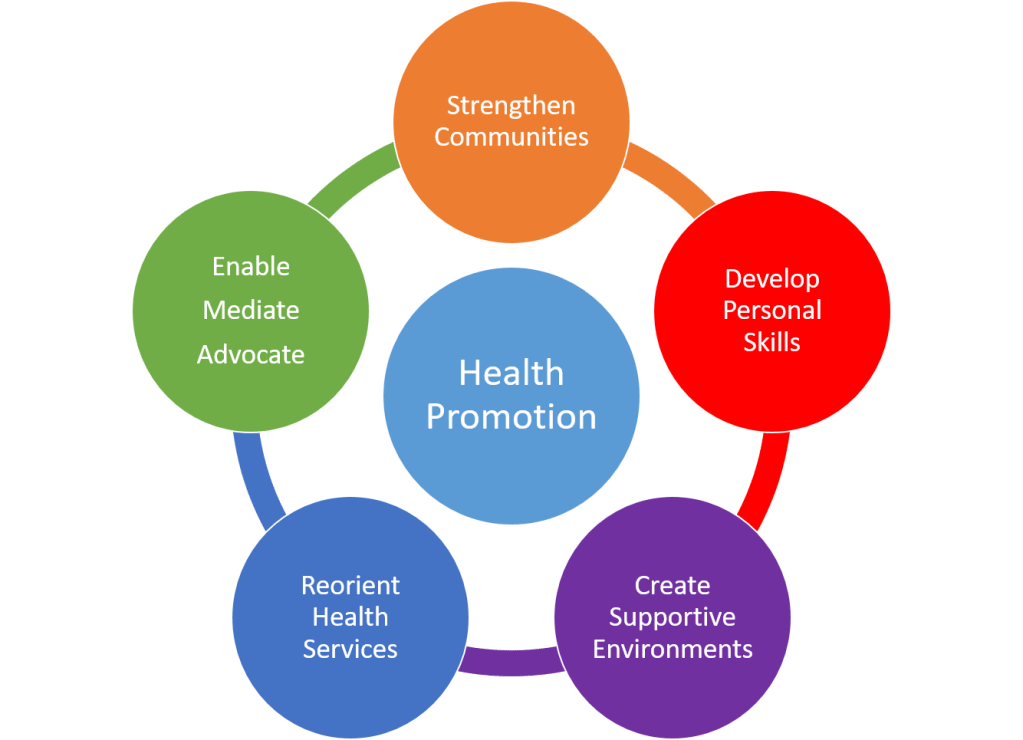
While following strategy in their favor like:
https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html
https://www.cdc.gov/reproductivehealth/maternalinfanthealth/severematernalmorbidity.html
http://www.ncbi.nlm.nih.gov/pubmed/18385496
https://wcms-wp.cdc.gov/hearher/maternal-warning-signs/index.html
Empower women
That Women and girls receive education on where to access maternal health care or seek remedies when they are denied care or their rights are otherwise violated, for those who live providing refugee camps with the resources to turn any place of accidental childbirth into a clean place, safe and fully equipped health facility,Safe delivery kits contain all the health products needed to give birth, the most marginalized women continue to experience high rates of maternal mortality.
In some countries child marriage has a lot to do with
Adolescent girls are exposed to increased rates of child marriage in crisis situations, children who do not experience any and their bodies are not mature enough to sustain pregnancy and ultimately increase the percentage of maternal deaths.
Help mothers understand the postpartum moment and its causes.
Post-partum depression is depression that occurs after having a baby, feeding postpartum depression are more intense and last longer than those of “baby blues,” a term used to describe the worry, sadness, and fatigue that many women feel after having a baby.
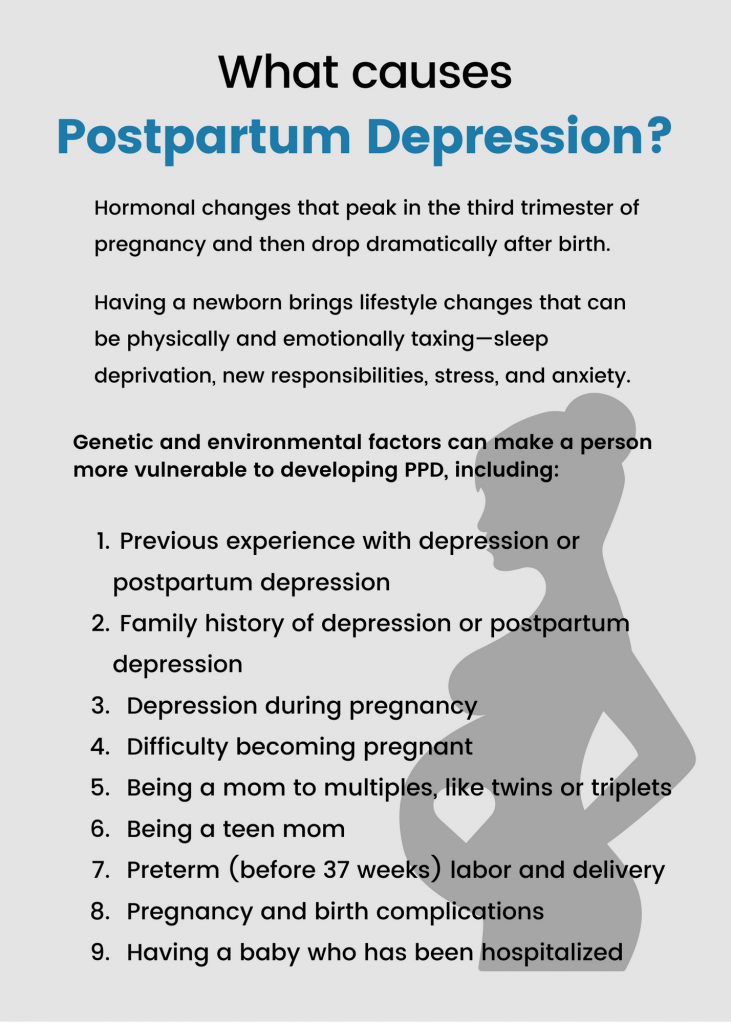
Everyone feels sad sometimes, but these feelings usually go away within a few days. It’s another matter after childbirth, depression interferes with the mother’s daily life and can last for weeks or months at a time. Most mothers with help can improve their situation, even those with the most severe forms of depression can improve with treatment as well.
Postpartum depression: https://www.cdc.gov/reproductivehealth/features/maternal-depression/
Symptoms postpartum depression:://www.cdc.gov/reproductivehealth/Depression/#post
Use technology to help improve maternal health
with the aim of improving maternal and child health, take of the opportunities offered by developing advanced access to new technologies to improve people’s health through recommendations strategic.
Implementation
Telemedicine is an innovative way of technology to enhance the quality of maternal care, simplify their lives and find a faster helper depending on the case, especially women travelis not as easy, or go to the office doctor due inconvenience and remote midwives- women can receive trainings for labor enhancement, thus improving the quality of care provided to mothers, in addition, the teleconsultation treats cases separately, allowing the user to create profiles for each patient.
The Solution can carry this new technology:
• share patient information between midwives
• rationalize patient follow-up
• Improve communications between midwives and their local health centers for faster dispatch of medical records.
• connect to a mobile network, data is automatically transmitted to the national health information management system, which saves time.

Telemedicine: https://www.cdc.gov/phlp/publications/topic/telehealth.html
Improve the care chain
Through interventions aimed at limiting delays in access to health services
are to set up more accessible means of communication
such as: telephone, computers, tablets, video call or zoom,
radio and transport vehicles, to reduce the financial barrier (cost of transport) as well as fatigue for consultations which are not worth it, it is essential to use these means in good time.
While expanding experiences and organizing a health system such as strengthening collaboration between different levels of care or mobilizing community members (including traditional birth attendants) to seek their help in emergencies
so that they actively participate in activities and facilitating pregnancy monitoring and disease diagnosis (for example, accompanying women during transport or providing community vehicles for urgent transport of women and/or new -born).
Google Docs document H.C.C plan https://docs.google.com/document/d/1HQg6-Sj-py56MKOjUqIExvp8fh2uNtMRizb3OLtmO7g/edit?usp=drivesdk
Press-releases
https://marayamaternalhealthcares.car.blog/press-releases/
Poster
https://marayamaternalhealthcares.car.blog/poster__trashed-3/
Infographic
://marayamaternalhealthcares.car.blog/infographic/
Procast
https://marayamaternalhealthcares.car.blog/procast__trashed-2/
Social media strategy https://marayamaternalhealthcares.car.blog/social-media-strategy__trashed-2/
Video PSA
https://marayamaternalhealthcares.car.blog/video-psa-2
Workshop
https://marayamaternalhealthcares.car.blog/workshop-2/